How Accurate Pupil Evaluation Enhances Post-Trauma Care?
The evaluation of the pupil diameter and its responsiveness is one of the critical criteria in the assessment of an individual’s neurological status. The accurate measurement of the pupils can provide great cerebral functioning insight, thereby leading to early diagnosis and therapeutic interventions. With advances in technology that have further improved the accuracy of pupil evaluation, healthcare providers are now more equipped to provide care for patients who have been admitted with traumatic injuries.
Importance of Pupil Assessment in Managing Trauma Ends
Pupil assessment forms a particularly fundamental component of the neuro exam, especially when trauma is suspected. Alterations in pupil size or their response can be suggestive of various neurological abnormalities due to cerebral edema, increased intracranial tension, or even TBI. For instance, a fixed or dilated pupil may indicate significant damage to the brain or damage to the cranial nerves, whereas unequal pupils may represent localized trauma.
In the context of post-trauma, the accurate and timely measurement of pupil reaction assumes increased significance. Measuring pupil diameter accurately helps clinicians monitor changes in neurological status and respond promptly to potential complications. Standardized methods and state-of-the-art technologies can now enable healthcare professionals to enhance the consistency and reliability of their assessments and eventually promote better patient outcomes.
Progress in Neurotechnological Tools
The traditional pupillary evaluation has widely changed with the incorporation of neurological tools. Such methods are subjective in nature and mostly vary, primarily because pupil measurements are done manually using a ruler or penlight. Modern devices such as digital pupillometers have become objective and accurate for pupil size quantifications and pupil responses.
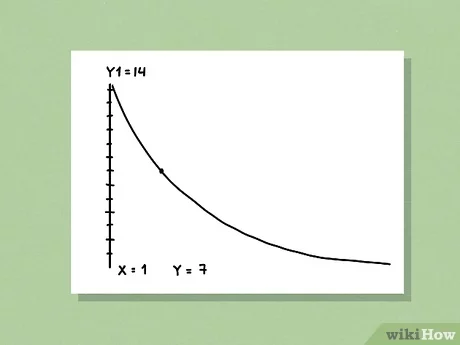
These high-tech devices enable lightning-fast assessment of pupillary responses in different lighting conditions, thus providing healthcare professionals with real-time feedback during neuro exams. One of the innovations in this domain is the Neurological Pupil Index (NPi), which measures pupil reactivity in a standardized manner. The NPi delivers a numerical score by way of advanced algorithms, giving a sense of the pupil’s response to exposure to light. Standardization gives greater resolution to the measurements of pupils, making it easier to monitor patients over longer periods.
Improve Decision-Making in Management after Trauma
The proper pupil diameter measurement plays a critical role in influencing clinical decision-making within the context of post-trauma care. By employing objective metrics derived from neurological tools, healthcare professionals can enhance their decision-making concerning treatment approaches. For example, an abrupt alteration in pupil diameter or responsiveness may indicate an urgent requirement for interventions such as imaging assessments or surgical consultation.
Greater, repeated monitoring of pupil reactions helps medical practitioners understand the extent of changes caused by interventions. Improvement in pupil reaction towards treatment has shown results as an optimistic sign of the patient’s neurological recovery. Worsening in pupil activity may necessitate assessment or modification of the treatment intervention. This adaptive nature of care and treatment after a trauma ensures that medical care providers stay alert and responsive to changes occurring in a patient’s condition.
Importance of Measuring Pupil Diameter in Patient Outcome
Checking pupils involves a very important aspect of measurement to check size, which is directly related to how well patients are doing. Through new technology, doctors are in a position to see the size of the pupils and minor changes otherwise unnoticed. It is quite important in traumatic head injury cases because small changes can be very significant for health.
Also, good tests that check pupils regularly can help healthcare workers work together more. Because the measurements are the same, healthcare teams can share important information more easily, which leads to working together to provide care and better management for patients. This teamwork is very important in the complicated area of recovery after trauma where different specialists might be part of a patient’s care.
Conclusion
Crucial for the good care of any traumatized patient is proper pupil activity examination. This will often give valuable information to the doctor about a patient’s brain health. Neurological tools developments and techniques for probing the human brain have led to new measurements in pupil size and reactivity using electronic pupillometers and the Neurological Pupil Index by doctors. Emphasis on proper pupil measurement analysis may facilitate better clinical judgment among healthcare providers, bringing about better patient outcomes.